Upper airway stenosis presents a diagnostic and therapeutic challenge due to its often insidious nature, frequently misdiagnosed as asthma, bronchitis, COPD, or CHF. Its incidence varies, with neonatal subglottic stenosis reported at 0-2% and tracheal stenosis often linked to procedures like tracheostomy or intubation. Causes can be congenital or acquired, including trauma, infections, or neoplastic diseases, with associated comorbidities such as GERD/LPR, neurologic disorders, congenital heart disease, and genetic syndromes. Clinical classifications and presentations vary, encompassing conditions like laryngomalacia and subglottic hemangioma. Diagnostic tools include endoscopic evaluations, biopsies, and imaging modalities like CT or MRI scans. Management ranges from observation and medical therapies to surgical interventions, including endoscopic techniques like laser treatments and open procedures such as laryngotracheoplasty or cricotracheal resection. Stents, such as silicone or metallic ones, may be used to maintain airway patency but can cause complications like infection or granulation tissue. Innovative treatments, such as laryngeal transplants and tissue-engineered tracheal transplants, represent advancements in care.
FULL NOTES SLIDES FOR READING
Reading Instructions:
- Using Next Button: Click the "Next" button at the bottom of the in-frame slider to move to the next slide.
- On Touch Devices: Swipe from right to left to view the next slide.
- Full-Screen Mode: For the best experience, switch to full-screen mode.
FULL SLIDES OUTLINE
Stenosis of Larynx & Trachea
Introduction
Airway stenosisTherapeutic and diagnostic challenge
Insidious presentation
Many times misdiagnosed as asthma/bronchitis, COPD, CHF
Incidence & trend
Neonatal subglottic stenosis 0 - 2.0%
(Metaanalysis, n=544) (Walner et al.,2001)
Tracheal stenosis following
tracheostomy 0.6-21%
laryngotracheal intubation 6% to 21%
(Grillo et al.,1995)
Clinical anatomy
Contd…
Adult and infant larynx
Tracheal lengths and diameters
Bernoullie principle
Aetiology
Congenital
Supraglottis
Laryngomalacia
Glottis
Laryngeal web
Subglottis
Congenital subglottic stenosis
Subglottic hemangioma
Aetiology
Acquired
Laryngotracheal trauma – External
Internal
Infection
Chronic granulomatous disease
Collagen Vascular disease
Neoplastic disease
Extrinsic compression
Foreign body
Laryngomalacia
Laryngomalacia
Etiology
Unknown
Theories
Anatomic theory
Cartilaginous theory
Neurologic theory
Comorbidities
GORD/LPR (65–100%)
Neurologic Disease (20– 45%)
Secondary Airway Lesions (7.5 to 64%)
Congenital Heart Disease (10%)
Congenital Anomalies/Syndromes/Genetic Disorders (8–20%)
Spectrum of Disease
Mild disease
Moderate laryngomalacia
Severe laryngomalacia
Clinical presentation
Inspiratory stridor
Phonation- normal
Feeding difficulties, failure to thrive
Respiratory distress, cyanosis
Holinger’s Classification
Type 1: Anterior prolapse of arytenoid and corniculate cartilages
Type 2: Tubular epiglottis which curls on itself
Type 3: Anteromedial collapse of arytenoids
Type 4: Posterior prolapse of epiglottis
Type 5: Short aryepiglottic folds
Investigation
Contd…
90% casesNo intervention, Reassurance
Anti-reflux therapy
Surgical management
Endoscopic supraglottoplasty
Tracheostomy
Success rate 94% (Richter, 2008)
Laryngeal web
Congenital /Acquired
Vocal folds (Commonest)
Clinical presentation
Mild dysphonia
Significant airway obstruction
Stridor Posterior interarytenoid web
1/3rd children SAL, commonly subglottic stenosis
Anterior glottic webs
Endoscopic approach : Cold steel or CO2 laser
Open approach: Laryngofissure +
Web excision + keel placement
Contd…
Posterior glottic web
Open approach : laryngofissure + posterior costal chondral graft
Endoscopic techniques:
- CO2 laser posterior cordotomy +/- partial arytenoidectomy
- Mucosal advancement flaps
- Microtrapdoor flaps
- Vocal cord lateralization
- Botox injections
Subglottic haemangioma
Vascular malformation
Biphasic stridor
Barking cough
Normal or hoarse cry
Failure to thrive
Contd…
Rigid bronchoscopy
Biopsy
Plain radiographs of neck (asymmetric narrowing of subglottis)
Contd…
1. Observation Small lesions
Tracheostomy
2. Steroid injection Small or medium-sized lesions
3. Systemic Steroid Partial regression
4. Laser ablation CO2 and KTP lasers
5. Oral Propranolol
Subglottic & Tracheal Stenosis
Congenital tracheal stenosis
Membranous webs
Segmental stenosis
Whole organ stenosis
Management
Membranous web
- Endoscopic rupture and dilatation
- KTP laser excision & ballon dilatation
Long segment tracheal stenosis or cartilaginous stenosis
- Tracheal resection & anastomosis
- Slide tracheoplasty
Tracheomalacia
Localized/Generalized
Primary/ Secondary
Spontaneous recovery
Tracheomalacia
Mild tracheobronchomalacia - No intervention
Severe tracheobronchomalacia
- Long-term CPAP
- Internal or external stenting
- Segmental resection + cartilage grafting
Vascular compression
Ring
Sling
Paediatric subglottic stenosis
Congenital 5%
Acquired 95%
SGS in intubated neonates
1970s and 1980s: 0.9 % - 8.3 %
After 1983: < 4 %
After 1990: < 0.63 %
Incidence 11.3%
(Manica et al., Laryngoscope ,2013)
Definition
Normal subglottic lumen diameter
Full term 4.5-5.5 mm
Preterm 3.5 mm
Subglottic stenosis
Full term <4 mm
Preterm <3 mm
Congenital subglottic stenosis
Incomplete recanalization
Membranous or Cartilaginous
History of recurrent croup
Acquired subglottic stenosis
Majority due to long-term or prior intubation
Duration of intubation
ETT size, material
Number of intubations
Traumatic intubations
Movement of ETT
Infection
Pathogenesis
Pathogenesis
Clinical presentation
Prior intubation
Progressive SOB
Noisy breathing
Contd…
History
Intubation records
Past medical history
Diabetes
Cardiopulmonary disease
Reflux
Systemic steroid use
Contd…
Examination
Observe
Stridor or labored breathing
Retractions
Breathing characteristics on exertion
Voice quality
Other abnormalities
Investigations
Flexible nasopharyngolaryngoscopy
Rigid laryngoscopy, bronchoscopy
Oesophagoscopy
Pulmonary function tests
Cotton-Myer grading for Subglottic stenosis
Contd…
McCaffrey
Contd…
Lano Classification : Based on involvement of glottis, subglottis and trachea
Stage I – one subsite involved
Stage II – two subsites involved
Stage III – three subsites involved
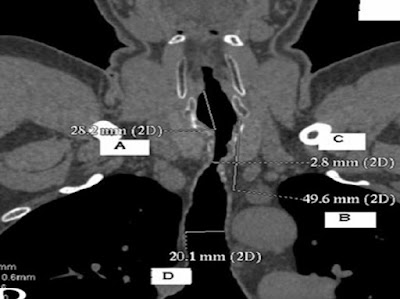
Radiological investigations
Plain films – Neck and chest
CT
MRI
Ultrasonography
Management
Medical
Observation
Tracheostomy
Endoscopic Treatment
Open procedure
Contd…
Medical
Diagnosis and treatment of reflux
Assess general medical status
Optimize cardiac and pulmonary function
Control diabetes
Discontinue steroid use before LTR
Contd…
Observation
Reasonable in mild cases
Repeat endoscopy every 3-6 monthly
Surgical Principles
Establish satisfactory airway
Decannulation
Preservation of laryngeal functions
Anaesthesia
Surgical modalities
Endoscopic approach
Dilation +/- stenting
Laser +/- stenting
Cryotherapy
Microcauterization
Excision of scar tissue
Contd…
Open procedure
Laryngotracheoplasty
Laryngotracheal reconstruction
Tracheal Resection with primary anastamosis
Endoscopic Approach
Less morbidity
Shorter hospital stay
Earlier return to work
Tolerance of repeated procedures
Contd…
Factors associated with failure
Previous attempts
Circumferential scarring
Loss of cartilage support
Exposure of cartilage
Arytenoid fixation
Combined LTS with vertical length >1cm
Endoscopic Dilatation
Multiple procedures
Lower success rate
Cannot undergo open procedures
CO2 Laser
Primary or as an adjunct
Re-epithelialization
Minimal deep tissue injury
Haemostasis
Preservation of mucosa
Contd…
Airway fire
Laser plume
Thermal injury
Laser excision of subglottic stenosis
Laser excision of subglottic stenosis
Contd…
Endoscopic laser treatment
CO2 laser radial incision
15% success
CO2 laser with steroid injection
18% success
CO2 laser with mitomycin-C topical application
75% success (Shapshay et al.,1998)
Microsurgical Debridement
Precise
Reduced injury to normal mucosa
less pain
Decreased operative time
External approach
Indications
Grades III and IV subglottic stenosis
Failed endoscopic management
Cicatricial scarring
Exposed perichondrium or cartilage
Combined laryngotracheal stenosis
External approach
Anterior cricoid split
Anterior Cricoid split & cartilage graft
Posterior Cartilage Graft
Anterior & posterior cricoid split & cartilage graft
Cricotracheal Resection
Indication
grade III & IV SGS
>3 mm margin between stenosis and vocal cords
CTR Contd…
CTR Contd..
CTR Contd..
Cricotracheal Resection
Acquired Tracheal Stenosis
Three types:
- Cicatricial
- Anterior wall collapse
- Complete stenosis
Management
Cicatricial tracheal stenosis
- CO2 laser excision
- Dilatation
Anterior wall collapse
- Augmentation with sternothyroid muscle or cartilage graft +Stent
Complete stenosis
- Tracheal resection & anastomosis
Tracheal resection & anastomosis
Tracheal resection
Tracheal resection
Neck flexion
Tracheal resection anastomosis
2-3 cm (4-6 rings)
Laryngeal resection maneuvers
Suprahyoid release
Infrahyoid release
Intrathoracic tracheal mobilization
Laryngeal release
Supra-hyoid release (Montgomery)
2-3 cm
Dysphagia
Laryngeal release
Infra-hyoid release (Dedo)
2.5 cm
Intrathoracic manoeuvres
Pulmonary ligament
Mainstem bronchus
Pericardial dissection
6.4 cm
Maintaining patency after laryngotracheal surgery
Stents
Keel
Mitomycin
Steroids
Scar Inhibitors
Mitomycin C
Antineoplastic and antiproliferative
5-FU & B-aminopropionitrile
Inhibit collagen cross-linking and scar formation
TGF-β
Contd…
Stenting
Ensure adequate airway during wound maturation
Prior to definitive resection/treatment
Palliation
Types of Stents
Laryngeal
Aboulker Stent
Montgomery LT-Stent
Laryngeal Keel
Types of Stents
SILICONE TRACHEAL STENT
Long-term tolerability
Easily removable
Poor mucocilary clearance
Can migrate
METALLIC TRACHEAL STENT
Incorporates into mucosa
Difficult to remove
Better mucociliary clearance
More reaction and granulation tissue
Tracheal Stents
Montgomery T-Tube
Healy Paediatric T-Tube
Eliachar LT-Stent
Monnier LT-Mold
Insertion of a T-tube
Complications
Local infection
Mucosal ulceration
Granulation tissue
Ischaemic mucosal injury
Recent advances
Laryngeal transplant
Kluyskens and
Ringoir (1969)
Strome et al.
(1998)
Contd…
Tissue-engineered tracheal transplant
(Baiguera et al., 2010)
THANK YOU